In the ongoing battle against sexually transmitted infections (STIs), clinicians face a persistent challenge: patients who become “lost to care.” These aren’t patients who choose to disappear, they are lost to stigma, systemic barriers, and logistical gaps that most clinics struggle to bridge. This can be particularly frustrating when trying to control the spread of disease in the community. With the Visby Sexual Health Test, providers can now meet patients where they are, offering timely answers and treatment in a single visit. It’s a breakthrough in accessibility that could redefine what’s possible in frontline STI care.
Lost-to-Care Patients Drive an Epidemic with Devastating Consequences
Currently, the United States is experiencing an alarming rise in STI cases. The Centers for Disease Control and Prevention (CDC) reports that one in five people in the U.S. has an STI, with about 26 million new cases diagnosed each year.1, 2 Notably, half of these new infections occur in young people aged 15-24, further highlighting the critical need for more effective intervention.3
But the human toll extends far beyond numbers. Untreated STIs lead to serious health consequences: higher risk of pelvic inflammatory disease (PID), infertility, and contracting HIV.4 The stakes are particularly high for women—50% of those who experience three episodes of PID become infertile.5 With untreated trichomoniasis, patients face a 2-3x higher risk of contracting other STIs, including HIV.6–9 The economic burden is equally staggering, with untreated STIs costing the health system $16 billion annually.3
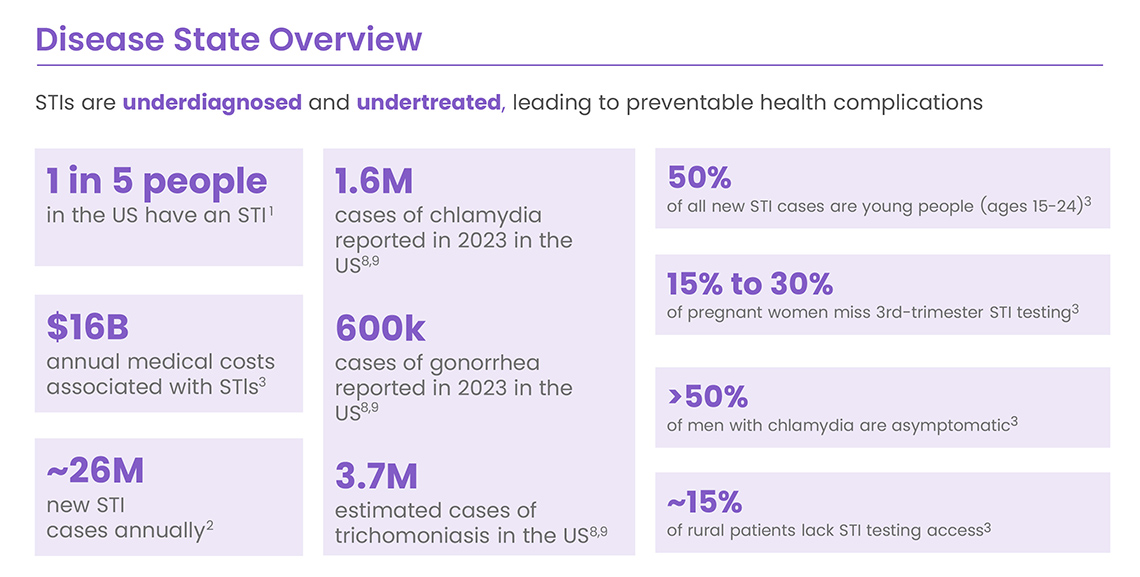
Yet many who need testing the most never receive it. Social stigma may keep patients from testing due to fear of judgment or embarrassment—even when symptoms are present. Educational gaps persist, with many unaware of STI risks or the necessity of regular testing, particularly for asymptomatic infections.4 Logistical barriers compound the problem: lack of transportation, inflexible work schedules, childcare responsibilities, and limited healthcare access in rural communities.3
Traditional STI Testing Workflows Fail When Patients Need Them Most
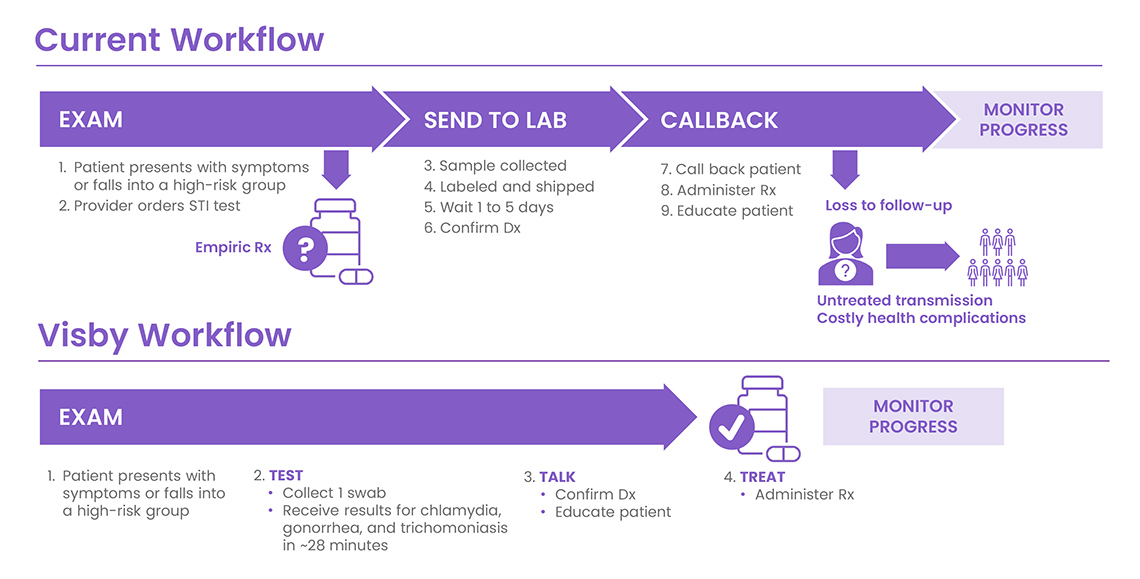
For clinicians, the lost-to-care problem can feel insurmountable because it’s beyond their direct control. They can’t provide transportation, change work schedules, or eliminate cultural stigmas. In addition, traditional diagnostic workflows only compound these challenges and can even work against them.
Current workflows have a fatal flaw – the wait. With 90% of STI testing sent to centralized labs, results don’t return for days.5 During this critical gap, 20-60% of patients who are left waiting for results disappear from care entirely5,6, the facility simply cannot reach them to communicate results and arrange treatment. Anticipating this inevitable loss, clinicians resort to empirical treatment, potentially contributing to antibiotic overuse and resistance.5
Even proactive measures fall short when required to wait for diagnostic results. Mobile outreach programs excel at reaching high-risk populations, but the days-long wait for test results makes it nearly impossible to complete treatment onsite. Screening high-risk patients during unrelated visits shows promise, but again, the delay between testing and results creates opportunities for patients to slip away.
Clinicians know the stakes are high, but they are working with tools that just don’t match the urgency of the problem.
From Lost-to-Care to Test-and-Treat with One Small Device
What if clinicians could seize an opportunity to test and treat STIs while a high-risk patient is being examined for another condition? Or if mobile outreach programs could not only intervene but resolve STI treatment right then and there? Or if stigma and anxiety could be alleviated with a promise of immediate and confidential results that attracts reticent STI patients to make an appointment?
Visby Medical has developed the Sexual Health Test that can circumvent the reliance on the traditional diagnostic workflow and deliver more immediate and actionable test results that enable clinicians to provide decisive and precise treatment – right then and there. The Visby Sexual Health test is a portable, single-use diagnostic device that delivers results in about 28 minutes and is the only CLIA-waived PCR STI test to provide results for the 3 most common and treatable STIs: chlamydia, gonorrhea, and trichomoniasis.7 Fitting in the palm of a clinician’s hand , the device only needs one vaginal sample swab for all three tests. By delivering PCR results right there and then when the patient is present, the Visby test can untether facilities from traditional diagnostic “send-out” testing.
Redesigning STI Care from the Bottom Up
One of the biggest challenges I see today is balancing the pace of innovation with real-world adoption. We’re seeing incredible advances in molecular diagnostics, digital health integration, and point-of-care solutions, but health systems often struggle to absorb these innovations due to entrenched workflows, reimbursement barriers, and a patchwork of regulatory expectations—especially in decentralized or at-home settings. By addressing diagnostic delays in STI care with point of care testing, we give clinicians the power to act swiftly, treat confidently, and break the cycle of untreated infections — especially with patients who could be lost to care. The question isn’t whether point-of-care STI testing will transform patient outcomes, it’s how quickly healthcare providers will adopt this game-changing technology to reclaim their lost-to-care patients.
References
- Sexually Transmitted Infections. Sexually transmitted infections prevalence, incidence, and cost estimates in the United States.Centers for Disease Control and Prevention website. Accessed April 2, 2025. https://www.cdc.gov/sti/php/communication-resources/prevalence-incidence-and-cost-estimates.html
- Addressing STI epidemics: integrating sexual health, intersectionality, and social determinants. In: National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on Prevention and Control of Sexually Transmitted Infections in the United States; Crowley JS, Geller AB, Vermund SH, eds. Sexually Transmitted Infections: Adopting a Sexual Health Paradigm. Washington (DC): National Academies Press (US); 2021.
- Sexually Transmitted Infection Statistics. Sexually transmitted infections surveillance, 2023. Centers for Disease Control and Prevention website. Accessed April 2, 2025. https://www.cdc.gov/sti-statistics/annual/index.html
- Malek AM, Chang CC, Clark DB, Cook RL. Delay in seeking care for sexually transmitted diseases in young men and women attending a public STD clinic. Open AIDS J. 2013 Jun 14;7:7-13. doi: 10.2174/1874613620130614002
- Garlock J, Lee L, Cucci M, Frazee LA, Mullen C. Suspected gonorrhea and chlamydia: Incidence and utilization of empiric antibiotics in a health system emergency department. Am J Emerg Med. 2019;37(5):884-889. doi: 10.1016/j.ajem.2018.08.015
- Huppert JS, Reed JL, Munafo JK, et al. Improving notification of sexually transmitted infections: a quality improvement project and planned experiment. Pediatrics. 2012 Aug;130(2):e415-22. doi: 10.1542/peds.2011-3326
- Visby Medical Sexual Health Test. Instructions for Use. 2025. Visby Medical.
- Sexually Transmitted Infection Statistics. National Overview of STIs in 2023. Centers for Disease Control and Prevention website. Accessed April 2, 2025. https://www.cdc.gov/sti-statistics/annual/summary.html
- Meites E. Trichomoniasis: the “neglected” sexually transmitted disease. Infect Dis Clin North Am. 2013;27(4):755-64. doi:10.1016/j.idc.2013.06.003
